Parkinson’s disease (PD) is one of the most devastating neurodegenerative conditions. Although dopamine replacement treatment or deep brain stimulation can give remarkable temporary benefit to many patients, there is still no cure and it is not yet possible to significantly slow the progression of the disease.
However, in recent years we have seen a remarkable progress in the understanding of the genetic, molecular and cellular underpinnings of the disorder, and new treatments may be within reach in the not too distant future.
Supported by a major private donation and research grants from the MJFF and EU worth more than 2,5 Million Euro, the Hertie Institute for Clinical Brain Research and the German Center for Neurodegenerative Diseases (DZNE) in Tübingen have established the Defeat Parkinson’s Research Platform. Clinical and pre-clinical researchers will be joining forces to use cutting edge molecular, genetic, cell biologic and computational technologies to better understand the complex mechanisms underlying the disorder and to develop novel biomarkers and treatments.
In the Defeat Parkinson’s Research Platform we will work together in an interdisciplinary team to explore how genetic variability leads to alterations in cellular and molecular processes that define disease risk and progression. To achieve this goal, we will join forces with our international collaborators (http://pdgenetics.org) to investigate the entire genomic variation in large groups of affected and at-risk individuals with next-generation sequencing technologies and correlate this data with transcriptome and epigenome information to build gene expression models. We will then explore how these changes alter cellular processes by high content/high throughput analysis, even at the single cell level, use novel computational approaches to integrate these findings in complex models. With our expert knowledge on disease modeling in induced pluripotent stem cells (iPSc) and animal models we will then investigate selected genes in depth and bring our knowledge back to our patients to discover and validate novel biomarkers and treatments.
Through the enthusiasm of our teams, with the input of numerous collaborators and the help of generous funders we are confident that we will make a difference to PD research and find new treatments that better the lives of our patients and eventually will lead to a cure or even prevention of PD.


Thomas Gasser is Professor of Neurology and director of the Department for Neurodegenerative Diseases at the HIH and the University Hospital for Neurology and heads the Parkinson’s Genetics group at the HIH and the DZNE Tübingen. He has led one of the teams discovering the LRRK2 gene as the most common cause for autosomal dominantly inherited PD and has, together with collaborators, pioneered GWA studies in PD. More information

Peter Heutink is head of the Genome Biology of Neurodegeneration group and speaker of the DZNE Tübingen. His team has identified genes causing inherited PD and risk loci for sporadic PD. His current interest focusses on the investigation of the molecular effects of the large number of risk genes identified for both familial and sporadic PD using high throughput genomic, bioinformatic and cellomic methods in induced Pluripotent Stem (iPS) cell models. More information

Philipp Kahle is head of the Functional Neurogenetics group at the HIH/DZNE Tübingen. Research aims at the understanding of neuropathological and epigenetics mechanisms of α-synuclein as well as mitochondrial quality control mechanisms regulated by recessive PD genes. More information

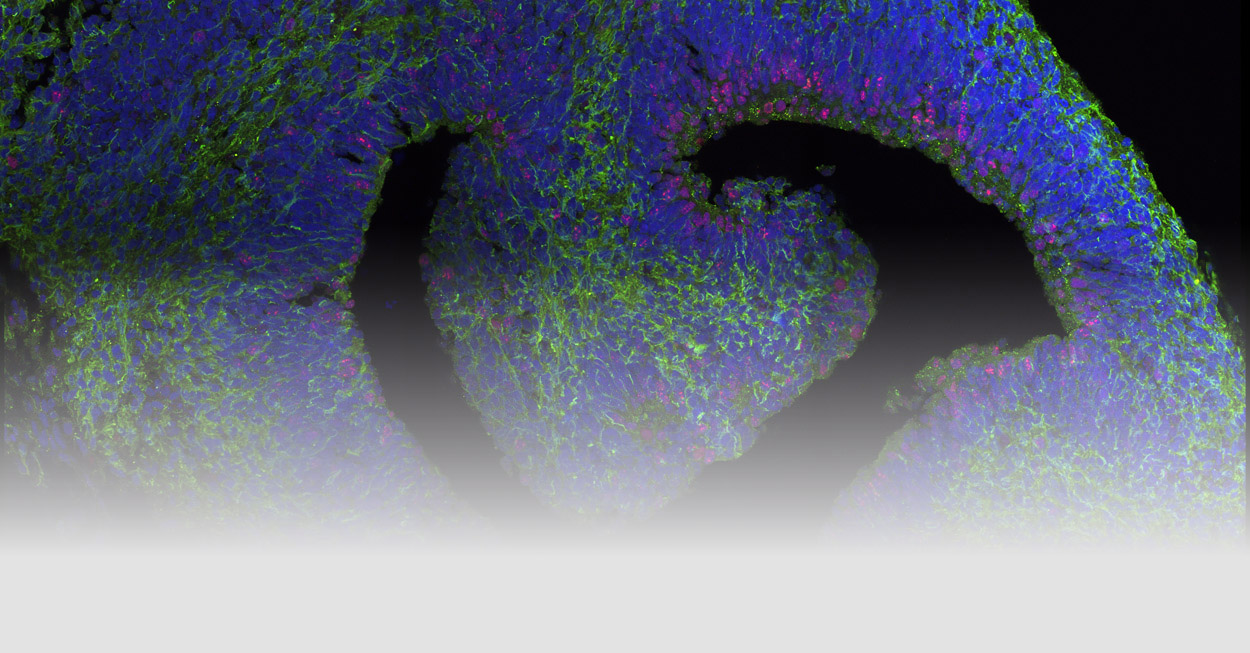
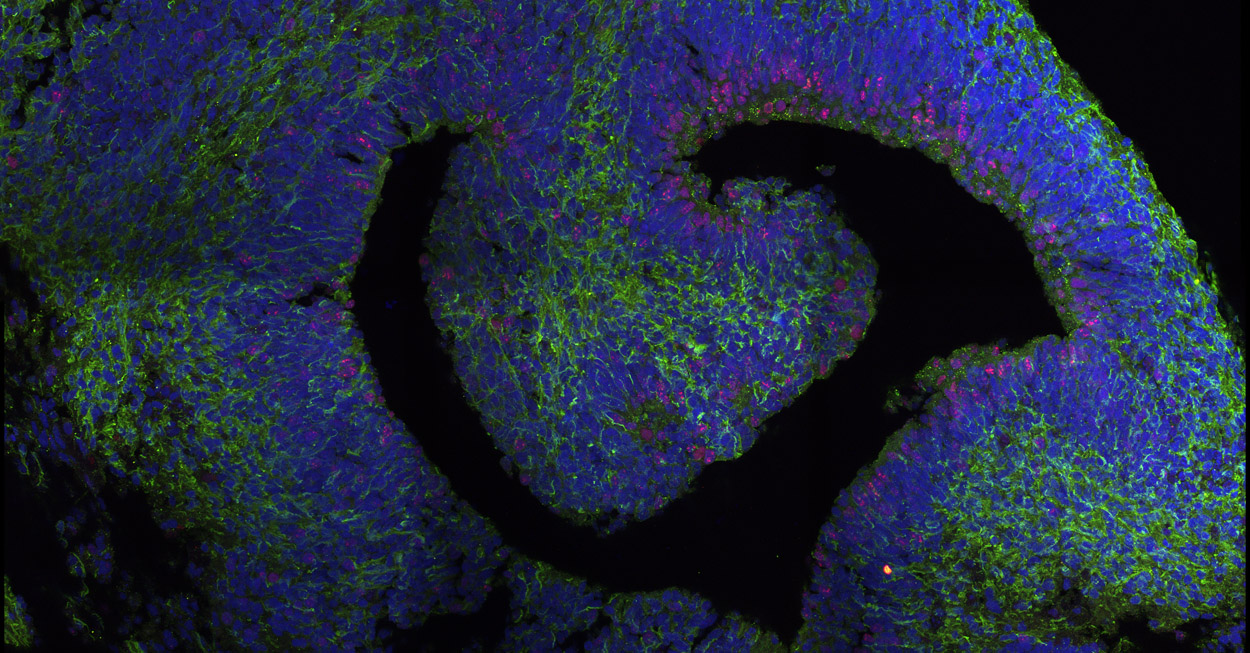
Michela Deleidi is a Helmholtz group leader at the DZNE-Tübingen and Junior Professor at the University of Tübingen. Her team works on the molecular mechanisms of neurodegeneration, with a special emphasis on the role of inflammation in Parkinson's disease. More information

Kathrin Brockmann heads the Parkinson’s disease outpatient unit at the Department of Neurology and is affiliated with the Integrated Clinical and Research Unit (ICRU) of the DZNE Tübingen. Her team focuses on patient stratification according to imaging patterns, genetic architecture and biomarkers as one of the major prerequisites to develop pathway-specific and milestone-related therapies. More information

Inga Liepelt-Scarfone is a neuropsychologist. As head of the Integrated Clinical and Research Unit (ICRU) of the DZNE Tübingen, she is responsible for a seemless workflow in numerous clinical trials. She also runs studies on cognitive and behavioural interventions in PD.

Julia Fitzgerald is a junior group leader at the Hertie-Institute for Clinical Brain Research, Tübingen working on the biological processes underlying neuronal cell death in Parkinson’s disease. Using genetic models and patient derived cells, the group focus on biochemical signaling and have a long standing specialism in mitochondria and the role of mitochondrial proteins in Parkinson’s disease.

Christian Johannes Gloeckner is group leader at the DZNE Tübingen. His team is working on the functional analysis of the PD-associated proteins. The current focus of the work is on the functional analysis of LRRK2 by systematic mapping of protein-interaction networks, by biochemical methods as well as by structural modelling. More information
Brockmann K, Lerche S, Dilger SS, Stirnkorb JG, Apel A, Hauser AK, Liepelt-Scarfone I, Berg D, Gasser T, Schulte C, Maetzler W: SNPs in Abeta clearance proteins: Lower CSF Abeta1-42 levels and earlier onset of dementia in PD. Neurology 2017, 89:2335-2340.
Brockmann K, Hilker R, Pilatus U, Baudrexel S, Srulijes K, Magerkurth J, Hauser AK, Schulte C, Csoti I, Merten CD, et al: GBA-associated PD. Neurodegeneration, altered membrane metabolism, and lack of energy failure. Neurology 2012, 79:213-220.
Brockmann K, Srulijes K, Hauser AK, Schulte C, Csoti I, Gasser T, Berg D: GBA-associated PD presents with nonmotor characteristics. Neurology 2011, 77:276-280.
Casadei N, Sood P, Ulrich T, Fallier-Becker P, Kieper N, Helling S, May C, Glaab E, Chen J, Nuber S, Marcus K, Rapaport D, Ott T, Riess O, Krüger R, Fitzgerald JC. (2016). Mitochondrial defects and neurodegeneration in mice overexpressing wild type or G399S mutant HtrA2. Human Molecular Genetics. 25(3):459-71.
Deleidi M, Jäggle M and Rubino R. "Immune ageing, dysmetabolism and inflammation in neurological diseases". Frontiers in Neuroscience. Front Neurosci. 2015 Jun 3;9:172. doi: 10.3389/fnins.2015.00172.
Fitzgerald JC, Zimprich A, Carvajal Berrio DA, Schindler KM, Maurer B, Schulte C, Bus C, Hauser AK, Kübler M, Lewin R, Bobbili DR, Schwarz LM, Vartholomaiou E, Brockmann K, Wüst R, Madlung J, Nordheim A, Riess A, Martins LM, Glaab E, May P, Schenke-Layland K, Picard D, Sharma M, Gasser T, Krüger R. (2017). Metformin reverses TRAP1 mutation-associated alterations in mitochondrial function in Parkinson’s disease. BRAIN: 140; 2444–2459.
Fitzgerald JC, Plun-Favreau H. (2008) Emerging pathways in genetic Parkinson’s disease: autosomal-recessive genes in Parkinson’s disease—a common pathway? FEBS Journal. 275(23), 5758-66.
Geisler, S., Holmström, K. M., Skujat, D., Fiesel, F. C., Rothfuss, O. C., Kahle, P. J., and Springer, W. (2010). PINK1/Parkin-mediated mitophagy is dependent on VDAC1 and p62/SQSTM1. Nat. Cell Biol. 12, 119-131
Gloeckner CJ, Kinkl N, Schumacher A, Braun RJ, O'Neill E, Meitinger T, Kolch W, Prokisch H, Ueffing M. The Parkinson disease causing LRRK2 mutation I2020T is associated with increased kinase activity. Human molecular genetics. 2006;15(2):223-32. doi 10.1093/hmg/ddi439
Guaitoli G, Raimondi F, Gilsbach BK, Gomez-Llorente Y, Deyaert E, Renzi F, Li X, Schaffner A, Jagtap PK, Boldt K, von Zweydorf F, Gotthardt K, Lorimer DD, Yue Z, Burgin A, Janjic N, Sattler M, Versees W, Ueffing M, Ubarretxena-Belandia I, Kortholt A, Gloeckner CJ. Structural model of the dimeric Parkinson's protein LRRK2 reveals a compact architecture involving distant interdomain contacts. Proceedings of the National Academy of Sciences of the United States of America. 2016;113(30):E4357-66. doi 10.1073/pnas.1523708113
Jansen IE, Ye H, Heetveld S, Lechler MC, Michels H, Seinstra RI, Lubbe SJ, Drouet V, Lesage S, Majounie E, Gibbs JR, Nalls MA, Ryten M, Botia JA, Vandrovcova J, Simon-Sanchez J, Castillo-Lizardo M, Rizzu P, Blauwendraat C, Chouhan AK, Li Y, Yogi P, Amin N, van Duijn CM; International Parkinson Disease Consortium, Heutink P. Discovery and functional prioritization of Parkinson's disease candidate genes from large-scale whole exome sequencing. Genome Biol. 2017 Jan 30;18(1):22. doi: 10.1186/s13059-017-1147-9.
Khurana V, Peng J, Chung CY, Auluck PK, Fanning S, Tardiff DF, Bartels T, Koeva M, Eichhorn SW, Benyamini H, Lou Y, Nutter-Upham A, Baru V, Freyzon Y, Tuncbag N, Costanzo M, San Luis BJ, Schöndorf DC, Barrasa MI, Ehsani S, Sanjana N, Zhong Q, Gasser T, Bartel DP, Vidal M, Deleidi M, Boone C, Fraenkel E, Berger B, Lindquist S. "Genome-scale networks link neurodegenerative disease genes to alpha-synuclein through specific molecular pathways". Cell Syst. 2017 Jan 25. pii: S2405-4712(16)30445-8. doi: 10.1016/j.cels.2016.12.011.
Mittal S, Bjørnevik K, Im DS, Flierl A, Dong X, Locascio JJ, Abo KM, Long E, Jin M, Xu B, Xiang YK, Rochet JC, Engeland A, Rizzu P, Heutink P, Bartels T, Selkoe DJ, Caldarone BJ, Glicksman MA, Khurana V, Schüle B, Park DS, Riise T, Scherzer CR. β2-Adrenoreceptor is a regulator of the α-synuclein gene driving risk of Parkinson's disease. Science. 2017 Sep 1;357(6354):891-898.
Piccoli G, Onofri F, Cirnaru MD, Kaiser CJ, Jagtap P, Kastenmuller A, Pischedda F, Marte A, von Zweydorf F, Vogt A, Giesert F, Pan L, Antonucci F, Kiel C, Zhang M, Weinkauf S, Sattler M, Sala C, Matteoli M, Ueffing M, Gloeckner CJ. Leucine-rich repeat kinase 2 binds to neuronal vesicles through protein interactions mediated by its C-terminal WD40 domain. Mol Cell Biol. 2014;34(12):2147-61. doi 10.1128/MCB.00914-13
Robak LA, Jansen IE, van Rooij J, Uitterlinden AG, Kraaij R, Jankovic J; International Parkinson’s Disease Genomics Consortium (IPDGC), Heutink P, Shulman JM; IPDGC Consortium members; International Parkinson’s Disease Genomics Consortium (IPDGC). Excessive burden of lysosomal storage disorder gene variants in Parkinson's disease. Brain. 2017 Nov 13. doi: 10.1093/brain/awx285. [Epub ahead of print]
Rotermund, C., Truckenmüller, F. M., Schell, H., and Kahle, P. J. (2014) Diet-induced obesity accelerates the onset of terminal phenotypes in a-synuclein transgenic mice. J. Neurochem. 131, 848-858
Schöndorf DC, Aureli M, McAllister FE, Hindley CJ, Mayer F, Schmid B, Sardi SP, Valsecchi M, Hoffmann S, Schwarz LK, Hedrich U, Berg D, Shihabuddin LS, Hu J, Pruszak J, Gygi SP, Sonnino S, Gasser T*, Deleidi M *. "iPSC-derived neurons from GBA1-associated Parkinson's disease patients show autophagic defects and impaired calcium homeostasis". Nat Commun. 2014 Jun 6;5:4028. doi: 10.1038/ncomms5028.
Simon-Sanchez J., Schulte C., Bras J. M., Sharma M., Gibbs J. R., Berg D., Paisan-Ruiz C., Lichtner P., Scholz S. W., Hernandez D. G., Kruger R., Federoff M., Klein C., Goate A., Perlmutter J., Bonin M., Nalls M. A., Illig T., Gieger C., Houlden H., Steffens M., Okun M. S., Racette B. A., Cookson M. R., Foote K. D., Fernandez H. H., Traynor B. J., Schreiber S., Arepalli S., Zonozi R., Gwinn K., van der Brug M., Lopez G., Chanock S. J., Schatzkin A., Park Y., Hollenbeck A., Gao J., Huang X., Wood N. W., Lorenz D., Deuschl G., Chen H., Riess O., Hardy J. A., Singleton A. B., Gasser T. Genome-wide association study reveals genetic risk underlying Parkinson's disease. Nat Genet. 2009;41(12):1308-12.
Sugeno N, Jäckel S, Voigt A, Wassouf Z, Schulze-Hentrich J, Kahle PJ. (2016) α-Synuclein enhances histone H3 lysine-9 dimethylation and H3K9me2-dependent transcriptional responses. Sci Rep. 6, 36328
Zimprich A., Biskup S., Leitner P., Lichtner P., Farrer M., Lincoln S., Kachergus J., Hulihan M., Uitti R. J., Calne D. B., Stoessl A. J., Pfeiffer R. F., Patenge N., Carbajal I. C., Vieregge P., Asmus F., Muller-Myhsok B., Dickson D. W., Meitinger T., Strom T. M., Wszolek Z. K., Gasser T. Mutations in LRRK2 Cause Autosomal-Dominant Parkinsonism with Pleomorphic Pathology. Neuron. 2004;44(4):601-7.
Supported by a donation
in memory of
Dr. Eugen Dörzbach
A joint initiative
![]()
![]()











